New science reveals how the heart’s “little brain” could change the way we understand and treat pain.
When we think of pain, we usually imagine the brain lighting up, processing signals, and reacting to discomfort. For decades, neuroscience has focused on how the brain perceives and responds to pain. But a fascinating wave of research is changing that narrative — and putting the heart in the spotlight.
💓 The Heart Has a Brain of Its Own
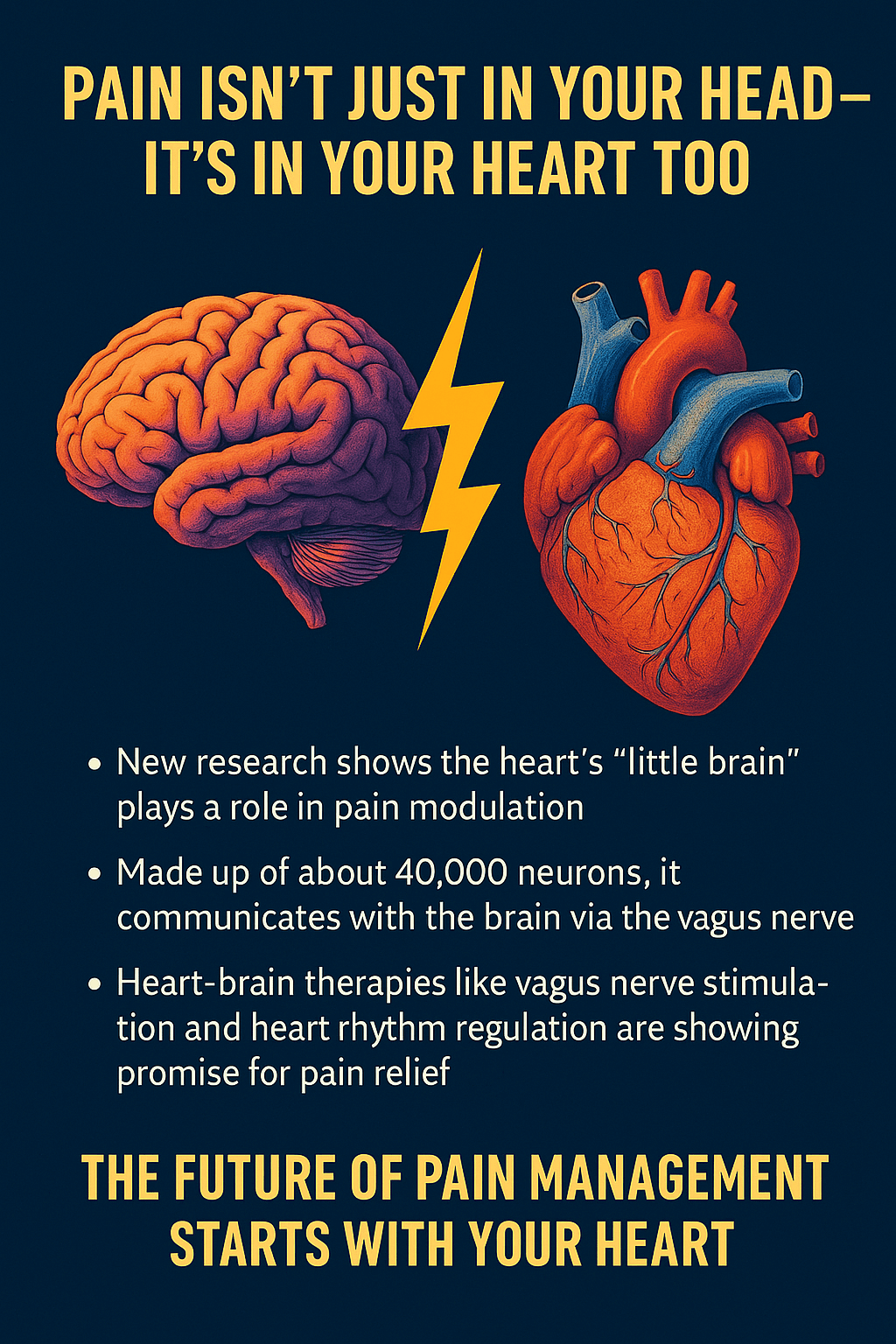
Known as the intrinsic cardiac nervous system, or the “heart brain,” this network of approximately 40,000 neurons operates semi-independently from the brain in your head. This neural system doesn’t just keep the heart pumping—it also communicates with your brain constantly through the vagus nerve, a powerful information superhighway in the body.
What’s more intriguing? The vagus nerve sends more signals from the heart to the brain than the other way around. That means your heart isn’t just a responder—it’s an active contributor in how you feel and process experience, including pain.
🧠❤️ Pain Is Not Just Neurological—It’s Emotional, Too
Research led by Dr. Ali M. Alshami highlights how the heart’s neural network plays a direct role in pain modulation. The brain doesn’t work alone when processing pain—it’s influenced by feedback from the heart, particularly in areas like:
- The amygdala (emotional memory and fear response)
- The cortex (thought, decision-making, awareness)
Pain, then, is a collaborative experience between the nervous system, the emotional body, and the heart. When you're in pain, your emotions, your breathing, and even your heart rhythm become active players in how you interpret it.
🔄 Heart-Brain Therapies: A New Frontier in Pain Relief
Therapies that regulate or harmonize the heart’s rhythm are showing promising results in managing chronic and emotional pain:
1. Vagus Nerve Stimulation (VNS):
Used in treatment for epilepsy and depression, VNS is now being studied for pain relief, especially for neuropathic and inflammatory pain.
2. Heart Rhythm Coherence (HRC):
Practices like heart-focused meditation, slow breathing, and biofeedback can shift your nervous system from “fight-or-flight” to “rest-and-repair,” reducing pain intensity and improving emotional regulation.
🌀 A Holistic View: Feeling Pain with Your Whole Being
Pain is no longer seen as just a signal traveling from body to brain. It’s a multi-dimensional experience—physiological, emotional, and even spiritual. The heart, with its intelligent rhythm and emotional resonance, is at the center of this experience.
So when you feel pain—whether physical or emotional—it’s not just “in your head.” Your heart is listening, responding, and sometimes even amplifying what you feel.
🌿 What This Means for You
- 🧘♀️ Start with breathwork: Deep, rhythmic breathing activates the vagus nerve and balances heart-brain communication.
- 🫀 Practice heart coherence: Spend a few minutes daily focusing on love, gratitude, or calm—this entrains your heart rhythms and reduces stress responses.
- 🎵 Use sound and vibration: Singing, chanting, and humming stimulate the vagus nerve and soothe the nervous system.
- 🛑 Reframe your approach to pain: Instead of suppressing pain, listen to it. What is your heart trying to say?
💬 Final Thoughts
Pain is not just a biological inconvenience—it’s a message from your inner world, asking to be heard and healed. And that message often originates from the rhythmic intelligence of your heart.
🩺 The future of pain management may not lie solely in medication or mental reframing.
It may begin with heart-based awareness, gentle breath, and the subtle wisdom of your body’s most powerful organ.
It may begin with heart-based awareness, gentle breath, and the subtle wisdom of your body’s most powerful organ.
Your heart isn’t just beating.
It’s speaking.
And healing may begin when you start listening.
It’s speaking.
And healing may begin when you start listening.


0 Comments